Progressive Focal Gray Matter Volume Loss in a Former High School Football Player: A Possible Magnetic Resonance Imaging Volumetric Signature for Chronic Traumatic Encephalopathy
Cyrus A. Raji1, M.D., Ph.D., David A. Merrill1, M.D., Ph.D., Jorge R. Barrio1, Ph.D., Bennet Omalu, M.D., M.P.H., Gary W. Small, M.D.
Received May 6, 2016; revised July 6, 2016; accepted July 15, 2016. From the Departments of Radiology (CAR); Psychiatry and Biobehavioral Sciences (DAM, GWS); Molecular and Medical Pharmacology (JRB), David Geffen School of Medicine at University of California, Los Angeles, CLA, Los Angeles, CA; and Department of Pathology (BO), University of California Davis Medical Center, Davis, CA. Send correspondence and reprint requests to Dr. Cyrus A. Raji, David Geffen School of Medicine at UCLA, Department of Radiology, 10751 Wilshire Blvd. Unit 608, Los Angeles, CA 90024. e-mail: cyrusraji@gmail.com
1 – These authors contributed equally to this work.
© 2016 American Association for Geriatric Psychiatry. Published by Elsevier Inc. All rights reserved. http://dx.doi.org/10.1016/j.jagp.2016.07.018
Case study
Here a case is presented of a 51-year-old former highschool football player with multiple concussions, including one episode with loss of consciousness. The patient experienced 6 years of cognitive and mood decline, and his wife corroborated increasing memory loss, attentional difficulties, and depressed mood without suicidal ideation.
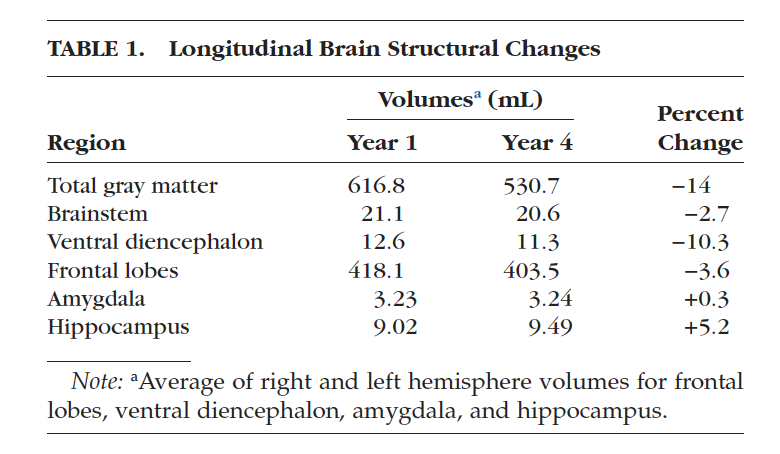
He had been unable to maintain fulltime employment because of progressive decline. Based on his presentation, he had been previously diagnosed with attention deficit hyperactivity disorder and bipolar disorder, type II. Neuropsychological tests indicated domain-specific cognitive impairment, and longitudinal volumetric magnetic resonance imaging (MRI) of the brain showed progressive brainstem, diencephalic, and frontal lobe atrophy.
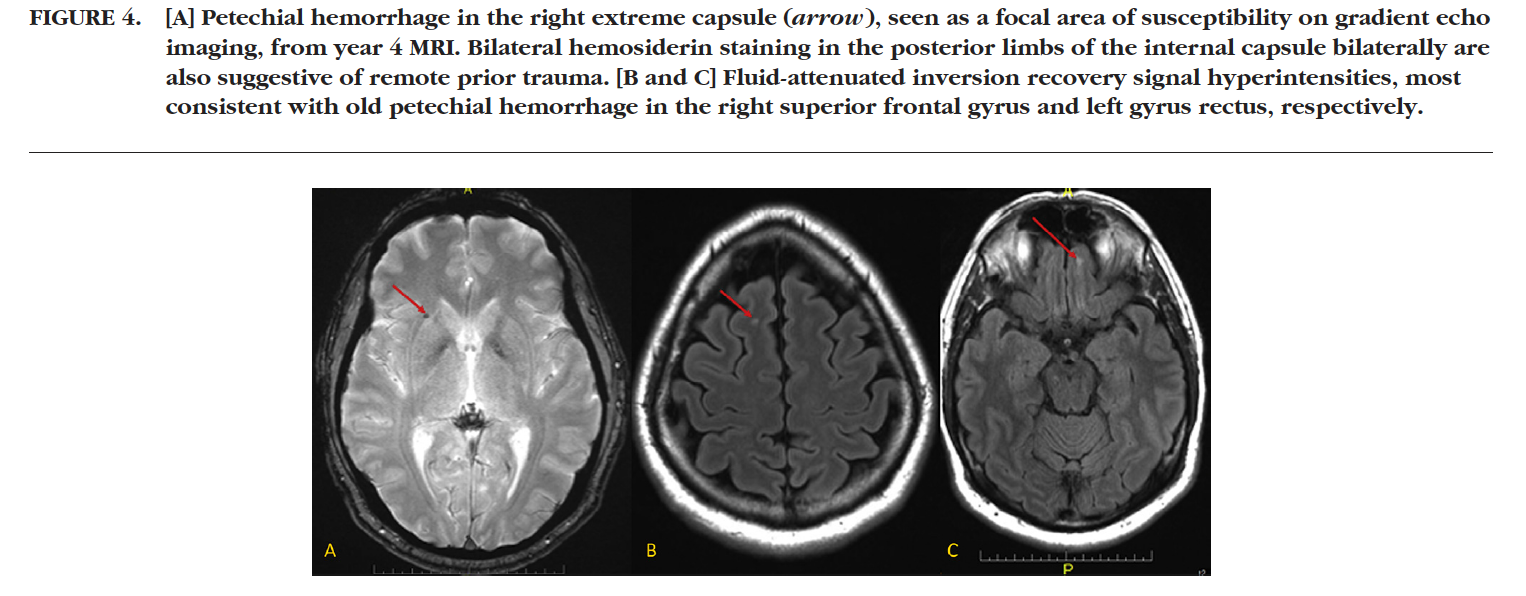
This regional volume loss correlated with the increased signal seen on tau and amyloid imaging (FDDNP-PET scan) of a separate case of suspected chronic traumatic encephalopathy (CTE). Visual assessment of the MRI also showed evidence of old petechial hemorrhages in the frontal and temporal-parietal lobe white matter. This case raises the possibility of distinct quantitative and visual brain MRI findings in suspected CTE.
Key Words: CTE, volumetric MRI, Neuroreader®, FDDNP, brain PET
Introduction
The relationship between American football and traumatic brain injury (TBI) has occupied an increasing focus in both the scientific literature and public discourse. Initial interest dates back almost a century to the description of the so-called punch drunk syndrome.1 Even comparatively recent literature has pointed to specific memory deficits in football players after concussions sustained on the field.2 However, it was only in the last decade where a pathologic basis for neuropathology related to contact sports— specifically football—was suggested with the description of chronic traumatic encephalopathy (CTE).3,4 Additional postmortem cases suggest that a potentially high percentage of professional football players may have CTE.5 Recent evidence also points to the presence of CTE in college football players, with at least one pathologically proven case in a 25-year old former college football player.6 Thus, although CTE has been predominantly described in former National Football League players, the presence of pathology in nonprofessional football players is largely unknown.
Concurrently, there has been developing interest in premortem diagnosis of CTE. Imaging has been a particularly powerful application, with positron emission tomography (PET) scans using 2-(1-{6-[(2-[F-18] fluoroethyl) (methyl)amino]-2-naphthyl}ethylidene)malononitrile (FDDNP) revealing high signals in the brainstem, amygdala, and orbital frontal cortex.7,8 These same brain region show high tau accumulation in autopsy cases of CTE. Diffusion tensor imaging has also suggested abnormalities in fractional anisotropy in patients with depression and anxiety after TBI.9 Volumetric magnetic resonance imaging (MRI) has shown promise in identifying regionally specific volume loss in TBI,10 but no known case examples are presented in the literature. MR volumetrics quantify the size of brain structures.
Currently, several U.S. Food and Drug Administration–cleared algorithms allow rapid, real-world quantification of clinical cases.11 One newer U.S. Food and Drug Administration–cleared algorithm, Neuroreader (Brainreader ApS, Horsens, Denmark),12 produces volumes of 45 different brain structures and shows agreement with manual hippocampal segmentation at both 1.5-T and 3.0-T field strengths. Here we describe the case of an individual with football related cognitive and psychiatric symptoms.We applied Neuroreader to longitudinal scans done 4 years apart.
The imaging and clinical findings are presented here followed by a contextual review of the literature.
Case presentation
Informed Consent
After an initial discussion with the patient and his wife, the case report was drafted, and the patient and his wife personally reviewed the contents, offering feedback for improvement. Subsequently, the patient met with two co-authors (C.R. and D.M.) to ask questions about the manuscript submission process and to review the results of the patient’s imaging, including the figures used for this report. Then, both the patient and his wife signed a consent form agreeing to the publication of this report with full understanding that they could retract such consent before publication. The UCLA Institutional Review Board was consulted regarding this report; however, the UCLA Institutional Review Board does not require approval of retrospective case studies involving less than three patients.
History of Present Illness
The patient is a 51-year-old married man without developmental problems or prior psychiatric history who presented to our cognitive health clinic in 2016 with an approximately one decade history of problems with mood lability, attention, and short-term memory. He also reported increased impulse control issues over this same period. He described having to “jumpstart” his brain each morning by playing online chess and/or exercising to avoid episodes described as “cognitive voids” during which he cannot think clearly, and it was hard for him to remember things. His wife corroborated this history, adding that the patient experienced increasing difficulty maintaining his job performance in sales over this time period because of progressive deficits in concentration. They presented to our cognitive health clinic seeking clarity on the cause(s) of his symptoms, his diagnoses, and estimation of his prognosis.
TBI History
The patient played football in high school for 3 years as a starting running back and defensive end. He was also a member of the special teams unit. Each of his three seasons consisted of approximately 10 games, plus full-contact practice 5 days a week from August through November (4 months per year). He went to a small high school; thus, he played “both ways,” starting on both offense and defense, plus participating in kickoffs and punt returns. Thus, he frequently played entire games without rest. During these games, he sustained multiple repetitive hits. As part of the patient’s high school football training, he was taught to go “head to head” in his play, projecting his head forward to absorb impacts. It was seen as a positive to have “a lot of nicks on your helmet from the opposing players.” He estimated that, on average, he would sustain half a dozen noticeable blows to the head per game (for example, a hard head-to-head hit during a play or hitting the ground hard when tackled). Each practice included an average of three hard hits to the head. Thus, an estimate of the total number of head impacts for the patient across his high school career is about 900 (180 during games, plus 720 during practices).
At age 17, he had at least one major concussion leading to loss of consciousness of unknown duration. This happened during an opening kick-off return. He was later told by his teammates that when he regained consciousness in the middle of the field, he got up and ran to the opponents’ sideline bench by mistake. Despite this error, he was not taken out of the game and in fact played the entire game. He recalled experiencing dissociative sensations during the game, as if he were “watching himself play.” That same week, the patient experienced headaches and difficulty sleeping but did not see a physician. Before high school the patient played junior “Pee Wee” football at age 12 for 1 year but did not recall any concussive episodes during this time. The patient also boxed recreationally with friends from ages 11 to 13 years, but he also did not recall any concussions or loss of consciousness during this activity. After high school, the patient was on his college team, but although he participated in summer training camps, he did not start in any college games.
Psychiatric and Medical History
The patient’s first psychiatric contact was in 2004 when he sought treatment after the onset of the symptoms described in the history of present illness (see above). Based on his presentation, he was given diagnoses of attention deficit hyperactivity disorder and bipolar disorder, type II. He did not have any childhood history of attention deficit hyperactivity disorder, any history of major depressive episodes or hypomania, or any history of psychiatric hospitalizations. The patient has not had any suicidal ideation or suicide attempts. He has a medical history of coronary artery disease status postplacement of two bare metal stents.
Social History
The patient had normal growth and development without learning disabilities. He did well in grade school and high school. The patient achieved 16 years of education and graduated from college with a degree in accounting. He has no history of military service. He had experienced a recent weight gain of 10 pounds and reported exercising several times per week with aerobics and strength training. According to the patient and his wife, he eats salmon two to three times a week, with flax and chia seeds. He is a non-smoker and has no history of drug or alcohol abuse.
Family History
There was a history of myocardial infarction and alcohol abuse in his father, who died when patient was 8 years old. The patient’s mother experienced intense emotional stress after the death of her husband but had no formal psychiatric diagnosis.
Medications
The patient takes dextroamphetamine/amphetamine salts for concentration, escitalopram and trileptal for mood, and memantine for cognition, as well as atorvastatin and clopidrogrel for coronary artery disease. The patient also takes vitamin B complex and omega-3 fatty acid supplements.
Laboratory Measurements
Routine blood work, including complete blood count, vitamin B12, and thyroid-stimulating hormone levels, did not show any abnormalities.
Neuropsychology Tests
Computerized neuropsychological testing13 revealed globally normal cognitive function with domainspecific abnormality of impaired executive function, including a Stroop test result14 in the 16th percentile. Memory performance was in the normal range (55th percentile).
Neuroimaging
The patient received two brain MRI scans, one in 2012 and one in 2016. Both scans were acquired with noncontrast T1-weighted three-dimensional magnetization-prepared rapid gradient-echo sequences on a 3-T MRI scanner. These images were then inputted into Neuroreader for volumetric analyses. Additional sequences included T2-weighted, fluidattenuated inversion recovery, and gradient echo imaging.
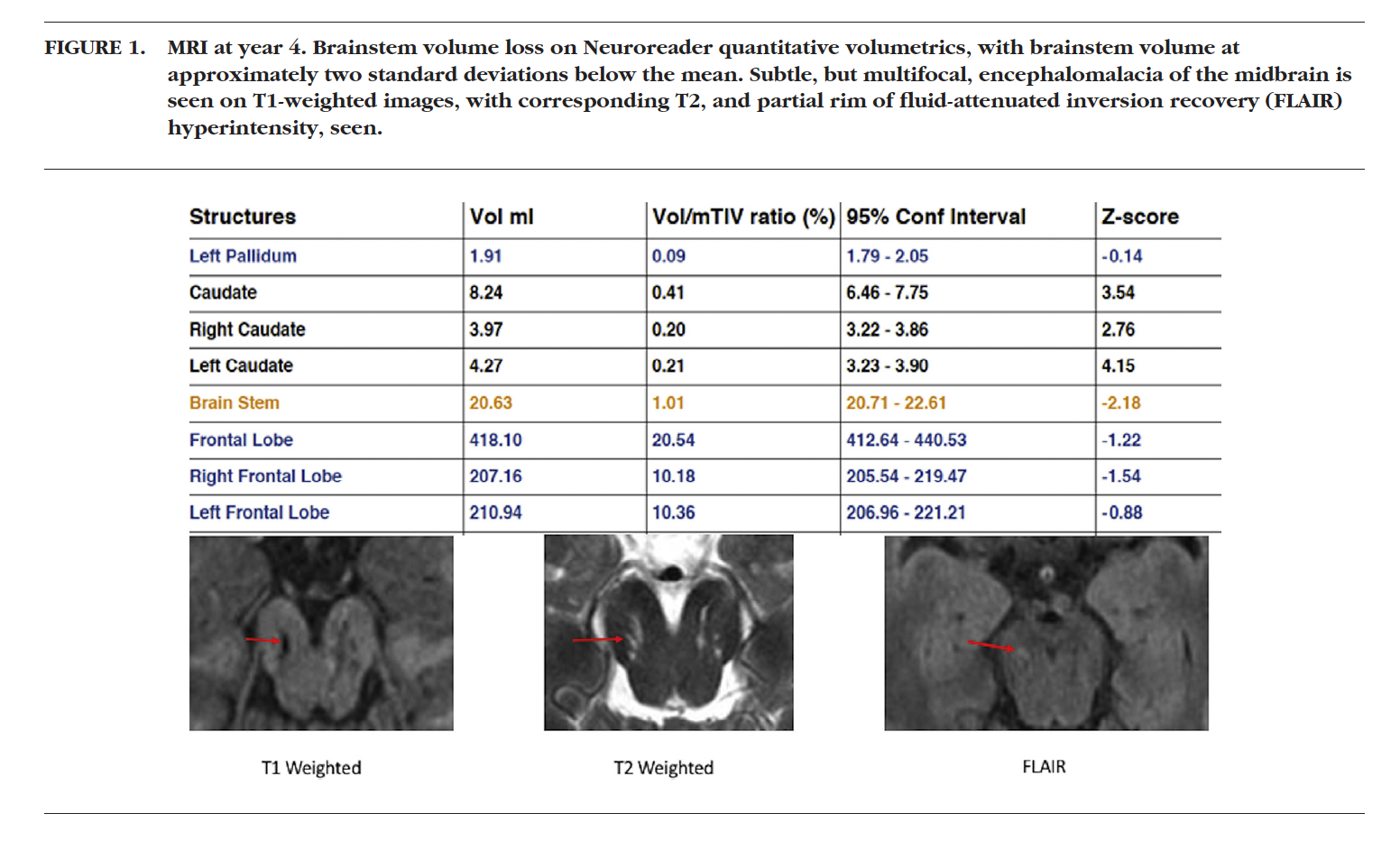
Figure 1 shows Neuroreader results with abnormally low brainstem volumes, approximately two standard deviations lower than the software control group mean. Visual inspection of the images indicated areas of T1 hypointense and T2 hyperintense foci of encephalomalacia in the midbrain of the brainstem, consistent with atrophy. One of the foci on the right showed a faint crescenteric focus of fluid-attenuated inversion recovery signal hyperintensity consistent with an old trauma.
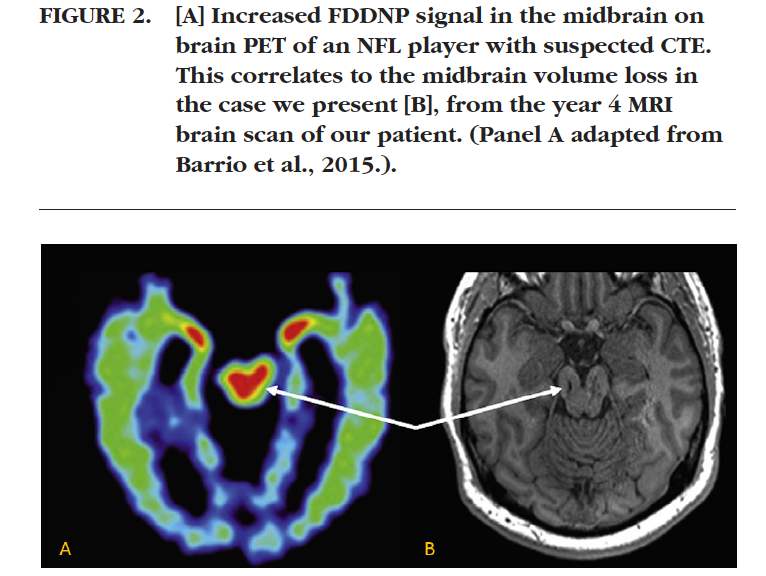
Figure 2 highlights the correlation between this regional atrophy and the known distribution of abnormally high signal on a separate case of suspected CTE, as imaged with the FDDNP-PET tracer.
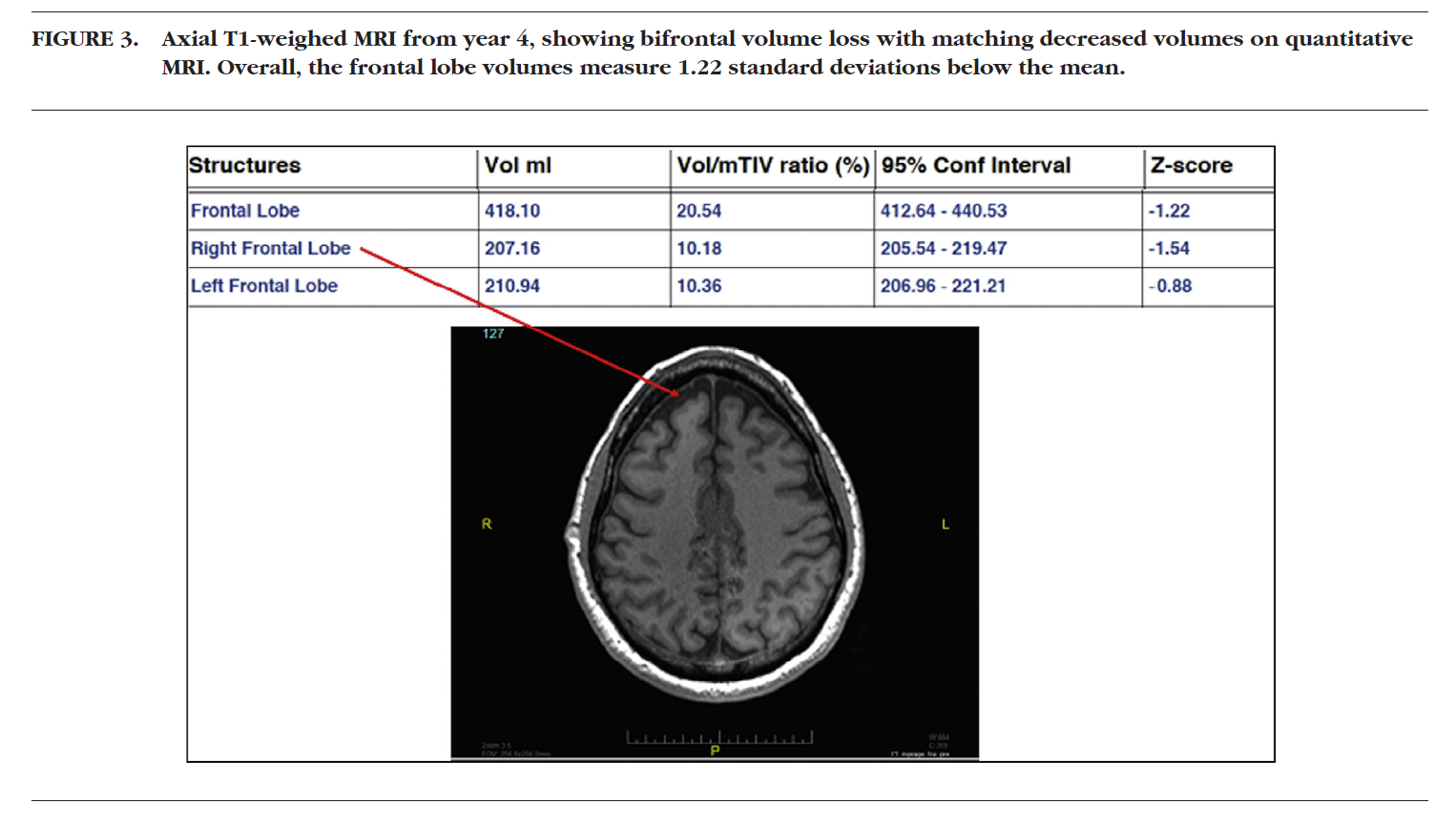
Figure 3 shows bifrontal volume loss with corresponding decreased mean volumes on Neuroreader output.
Progressive Focal Gray Matter Loss in a Former High School Football Player.
Figure 4 shows blood products from old trauma in the right deep frontal white matter and basal ganglia (A) and areas of gliosis in the right superior frontal gyrus and left gyrus rectus (B and C).
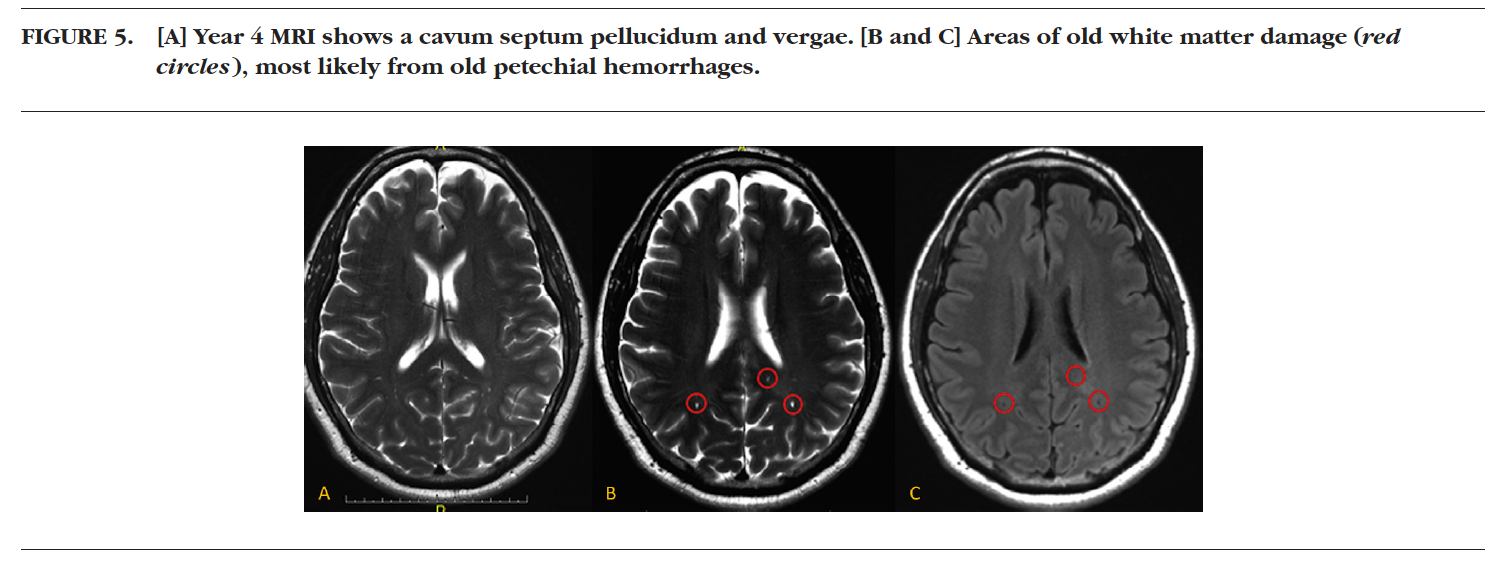
Figure 5 shows images of a cavum septum pellucidum and small foci of volume loss in the parietal-temporal white matter.
Table 1 shows the longitudinal structural changes over the 4 years between the two MRI scans. Total gray matter volume decreased by 14%, with the largest decreases seen in the midbrain, ventral diencephalon, and the frontal lobes. The patient did not have any volume loss in either the temporal or parietal lobes. No other areas of abnormally low volumes were calculated.
Discussion
This case documents what may be the first known example of longitudinal regional atrophy in a former high school football player with suspected CTE. Because a definitive diagnosis of CTE can only be made by autopsy, the patient’s diagnosis remains uncer tain, but the history, progressive cognitive and mood decline, along with longitudinal brain atrophy make the possibility of CTE likely. Other supportive information is the correlation between the most severe regional volume loss and known areas of increased FDDNP-PET signal in a separate suspected case of CTE, which is consistent with multiple other reports, as well as regions of tau accumulation in autopsy-confirmed cases of CTE.7,8
The longitudinal progression of atrophy is also in keeping with knowledge of CTE as a neurodegenerative process. The fact that hippocampal atrophy was not demonstrated in the patient scan is reassuring that the patient does not suffer from Al- zheimer dementia.15 The normal temporal lobes are also strongly suggestive that the patient does not suffer from frontotemporal dementia.16 The combination of both psychiatric and executive function deficits is in keeping with the known symptoms of CTE17 and matches the frontal lobe atrophy seen both qualitatively and quantitatively in this patient. It is also important to note the sensitivity of volumetric MRI for detecting atrophy with longitudinal scans.18
An additional MRI finding supporting possible CTE is a cavum septum pellucidum, a finding that, although itself nonspecific, has been seen in persons with CTE with a history of contact sports.19 Although the patient was given a presumptive bipolar disorder diagnosis, volume loss associated with this disorder has been reported in the hippocampus and cerebellum,20 both of which showed normal volumes in this patient. The normal hippocampal volume is consistent with the patient’s preserved memory function and healthy lifestyle behaviors, such as fish consumption and physical exercise.21 Additionally, the lack of amygdala atrophy is consistent with absence of suicidal ideation or attempts, as well as adequate treatment of psychiatric symptoms from any concussion-related brain damage. Indeed, prior research suggests that football-related head trauma may be potentially reversed with a comprehensive treatment approach.22
The findings of this one case report are preliminary. Additional studies, with comparisons with a control group, are required to see if these MRI findings apply at a group level. Additionally, correlation with amyloid and tau imaging is important, although such methods are not part of standard clinical practice.
However, if replicated, these findings may constitute a specific MR volumetric signature of CTE. Volumetric MRI is also important for ruling out other conditions such as Alzheimer disease and frontotemporal dementia. The idea of reform in football is not new. In 1904, 18 college football players died from field play and 159 were seriously injured, leading to new rules suggested by President Theodore Roosevelt himself for safer play and the eventual creation of the National Collegiate Athletic Association to protect players.23
Ongoing attempts to enact new concussion protocols are vital in the protection of players at all levels, from high school to college to the professional level. Our work, taken together with prior literature, suggests that additional protection for football players at all levels is critical. Because contact sports such as football continue to be played, serious consideration will need to be rendered regarding applying quantitative imaging, neuropsychology testing, and functional medical assessments at baseline and follow-up for contact sport participants to successfully identify and treat those suffering from TBI and suspected CTE.
Am J Geriatr Psychiatry October 2016; 24:784–790
Special acknowledgment is reserved for M. Reza Raji, M.D., M.P.H., for his separate external editorial feedback. Drs. Barrio, Omalu, and Small have financial interests in TauMark, LLC, which has licensed the [F-18]FDDNP patents from UCLA. Dr. Raji consults for the Change Your Brain Change Your Life and Brainreader ApS. Dr. Merrill has no disclosures.
References
- Martland HS: Punch drunk. JAMA 1928; 91:1103–1107
- Yarnell PR, Lynch S: Progressive retrograde amnesia in concussed football players: observation shortly postimpact. Neurology 1970; 20:416–417
- Omalu BI, DeKosky ST, Minster RL, et al: Chronic traumatic encephalopathy in a National Football League player. Neurosurgery 2005; 57:128–134, discussion 128–134
- Omalu BI, DeKosky ST, Hamilton RL, et al: Chronic traumatic encephalopathy in a national football league player: part II. Neurosurgery 2006; 59:1086–1092, discussion 1092–1083
- Bieniek KF, Ross OA, Cormier KA, et al: Chronic traumatic encephalopathy pathology in a neurodegenerative disorders brain bank. Acta Neuropathol 2015; 130:877–889
- Mez J, Solomon TM, Daneshvar DH, et al: Pathologically confirmed chronic traumatic encephalopathy in a 25-year-old former college football player. JAMA Neurol 2016; 73:353–355
- Small GW, Kepe V, Siddarth P, et al: PET scanning of brain tau in retired national football league players: preliminary findings. Am J Geriatr Psychiatry 2013; 21:138–144
- Barrio JR, Small GW, Wong KP, et al: In vivo characterization of chronic traumatic encephalopathy using [F-18]FDDNP PET brain imaging. Proc Natl Acad Sci USA 2015; 112:E2039–E2047
- Alhilali LM, Delic JA, Gumus S, et al: Evaluation of white matter injury patterns underlying neuropsychiatric symptoms after mild traumatic brain injury. Radiology 2015; 277:793–800
- Ross DE,Ochs AL, Seabaugh J, et al: NeuroQuant(R) revealed hippocampal atrophy in a patient with traumatic brain injury.
J Neuropsychiatry Clin Neurosci 2012; 24:E33 - Brewer JB: Fully-automated volumetric MRI with normative ranges: translation to clinical practice. Behav Neurol 2009; 21:21–2
- Ahdidan J, Raji CA,DeYoe EA, et al: Quantitative neuroimaging software for clinical assessment of hippocampal volumes on MR imaging. J Alzheimers Dis 2015; 49:723–732
- Iverson GL, Brooks BL, Ashton Rennison VL: Minimal gender differences on the CNS vital signs computerized neurocognitive battery. Appl Neuropsychol Adult 2014; 21:36–42
- Stroop JR: Studies of interference in serial verbal reactions. J Exp Psychol 1935; 18:643–662
- Brueggen K, Dyrba M, Barkhof F, et al: Basal forebrain and hippocampus as predictors of conversion to Alzheimer’s disease in patients with mild cognitive impairment—a multicenter DTI and volumetry study. J Alzheimers Dis 2015; 48:197–204
- Boccardi M,Laakso MP,Bresciani L, et al:The MRI pattern of frontal and temporal brain atrophy in fronto-temporal dementia. Neurobiol Aging 2003; 24:95–103
- Maas A: Traumatic brain injury: changing concepts and approaches. Chin J Traumatol 2016; 19:3–6
- Ross DE:Review of longitudinal studies of MRI brain volumetry in patients with traumatic brain injury. Brain Inj 2011; 25:1271– 1278
- Costanza A,Weber K,Gandy S, et al:Contact sport-related chronic traumatic encephalopathy in the elderly: clinical expression and structural substrates. Neuropathol Appl Neurobiol 2011; 37:570–584
- Redlich R, Almeida JJ, Grotegerd D, et al: Brain morphometric biomarkers distinguishing unipolar and bipolar depression. A voxelbased morphometry-pattern classification approach. JAMA Psychiatry 2014; 71:1222–1230
- Raji CA, Erickson KI, Lopez OL, et al: Regular fish consumption and age-related brain gray matter loss.Am J Prev Med 2014;47:444– 451
- Amen DG,Wu JC,Taylor D,et al:Reversing brain damage in former NFL players: implications for traumatic brain injury and substance abuse rehabilitation. J Psychoactive Drugs 2011; 43:1–5
- Klein C:How Teddy Roosevelt Saved Football. 2012.
http://www.history.com/news/how-teddy-roosevelt-saved-football.
Accessed on April 24, 2016